Medically reviewed by Dr. Jordan Pinsker, Vice President & Medical Director, Tandem Diabetes Care.
Type 1 and type 2 diabetes both revolve around how the body does or doesn’t use insulin. In some instances, there is crossover between managing type 1 diabetes and type 2 diabetes.
For example, someone living with type 2 diabetes (insulin resistance) may try adjustments to diet, a change in lifestyle, or non-insulin medications to try and treat type 2 diabetes before moving directly to insulin.
Because type 1 diabetes (insulin dependence) is an autoimmune disease, it requires daily insulin therapy.
Learn more about the differences between type 1 and type 2 diabetes.
Someone living with type 1 diabetes has several options for their daily insulin therapy. They can administer insulin through injections, pens, inhaled insulin, or by using an insulin pump.
One of the major advancements in managing diabetes is using an automated insulin delivery (AID) system.
This article will provide an overview of automated insulin delivery and how it can benefit children or adults with type 1 diabetes. It will also give an overview of other ways to manage type 1 diabetes.
What is Automated Insulin Delivery?
One of the newest advancements for managing type 1 diabetes in children and adults is through the use of an automated insulin delivery system — also called an AID system. An automated insulin delivery system for managing diabetes is made up of three components — an insulin pump, a continuous glucose monitoring (CGM) sensor, and in some pumps an algorithm that can predict glucose levels and automatically dose insulin.
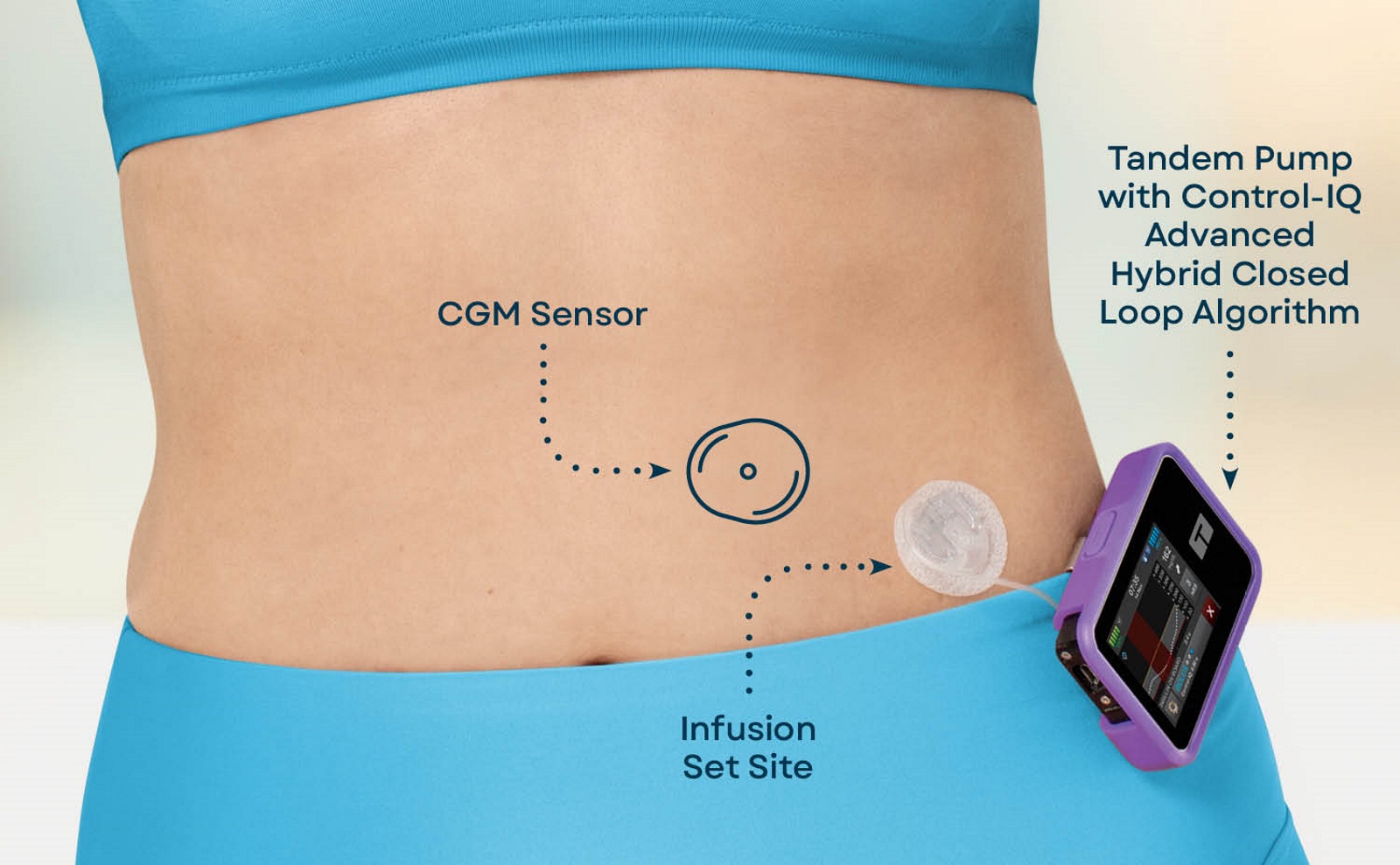
A CGM will deliver real-time glucose readings to the insulin pump via Bluetooth® connectivity. An algorithm — like the predictive software Control-IQ technology from Tandem Diabetes Care — will use those CGM sensor readings to determine whether to administer insulin or suspend insulin.
Sometimes this is referred to as a “closed-loop system.” It has also been referred to as an “artificial pancreas” because the system aims to mimic how the pancreas would adjust to glucose levels.
Learn more about insulin pumps with an advanced hybrid closed-loop system.
“Automated insulin delivery systems are constantly adjusting things in the background,” said Dr. Jordan Pinsker, Chief Medical Officer for Tandem Diabetes Care, who is also a renowned pediatric endocrinologist. “By doing this, the system can react far faster than a person and really reduce the burden of diabetes management. For example, the system can help you to get a good night’s sleep, so you don’t have to worry about your blood sugar all night long.”
This can be particularly helpful for sleeping with diabetes or for the parent of a child with type 1 diabetes.
Automated Insulin Delivery and Type 1 Diabetes
Type 1 diabetes is an autoimmune disease that attacks the cells in the pancreas that make insulin. It is typically diagnosed in childhood, which is why it used to be called juvenile diabetes. However, people of all ages can be diagnosed with type 1 diabetes.
Type 1 diabetes requires daily insulin therapy.
The goal of an AID system is to maximize the amount of time glucose levels are inside a target range of 70-180 mg/dL. This range is widely accepted as the target range by the American Diabetes Association guidelines for a non-pregnant individual.
Learn more about time in range and what it means for someone living with type 1 diabetes.
There are many factors that can influence the amount of time glucose is in range for someone living with diabetes — including the time of day, stress levels, or illness. The purpose of an automated insulin delivery system is to help offset some of these factors.
When glucose levels go outside of this target range someone with type 1 diabetes may experience hypoglycemia (lows) or hyperglycemia (highs).
Learn more about the differences between hypoglycemia and hyperglycemia — including the signs and symptoms of hypoglycemia or hyperglycemia — and what it means for someone living with diabetes.
“Technology to help people manage diabetes has advanced tremendously over the past 20 years,” said Dr. Pinsker. “Years ago, it was inconceivable that an insulin pump and a glucose sensor could talk with each other and automatically adjust insulin delivery every five minutes. Today, automated insulin delivery systems are recommended1 for all people with type 1 diabetes.”
Insulin Therapy for Type 1 Diabetes
/ ! \ Important: Always consult a healthcare professional for information about how to manage diabetes.
There are several different options for people with type 1 diabetes who need daily insulin therapy.
Daily Injections
One of the most common treatment options is multiple daily injections. This is sometimes called MDI insulin therapy.
Insulin pens
Similar to MDI therapy, insulin pens require multiple injections throughout the day and on an as-needed basis. Pens typically come with the insulin prefilled to help with dosing.
Insulin pump
An insulin pump gives a steady release of insulin (called a basal rate) throughout the day. It can also deliver a larger dose of insulin, called a bolus, that is initiated by the user prior to meals. When a pump has a CGM and a predictive algorithm, it can form an AID system.
Learn more about insulin and how it works.
About Tandem Diabetes Care
Tandem Diabetes Care makes the Tandem Mobi system and the t:slim X2 insulin pump. The predictive algorithm designed for use with these pumps, Control-IQ technology, can predict glucose levels up to 30 minutes in advance when paired with a CGM (sold separately) to help prevent highs and lows.
Tandem Mobi is the world’s smallest, durable automated insulin delivery system.1 The t:slim X2 is the #1 rated insulin pump and AID system.2
“Automated insulin delivery systems, such as the t:slim X2 insulin pump with Control-IQ technology, show immediate and sustained improvement in time in range, with benefits often seen after just one day of use.3 These benefits continue over time,” Dr. Pinsker explained.
Learn more about Tandem Mobi.
Learn more about the t:slim X2 insulin pump.
References
1. As of Nov., 2024. Data on file, Tandem Diabetes Care.
2. dQ&A US Patient Panel Q3 2023 (July-Sept. 2023).
3. Breton MD, Kovatchev BP. One year real-world use of the Control-IQ advanced hybrid closed-loop technology. Diabetes Technol Ther. 2021;23(9):601-608. doi: 10.1089/dia.2021.0097.
Important Safety Information
RX ONLY.
Indications for Use
Tandem Mobi system: The Tandem Mobi insulin pump with interoperable technology (the pump) is intended for the subcutaneous delivery of insulin, at set and variable rates, for the management of diabetes mellitus in persons requiring insulin. The pump is able to reliably and securely communicate with compatible, digitally connected devices, including automated insulin dosing software, to receive, execute, and confirm commands from these devices. The pump is intended for single patient, home use and requires a prescription. The pump is indicated for use in individuals 6 years of age and greater.
t:slim X2 insulin pump: The t:slim X2 insulin pump with interoperable technology is intended for the subcutaneous delivery of insulin, at set and variable rates, for the management of diabetes mellitus in people requiring insulin. The pump is able to reliably and securely communicate with compatible, digitally connected devices, including automated insulin dosing software, to receive, execute, and confirm commands from these devices. The pump is intended for single patient use. The pump is indicated for use with NovoLog or Humalog U-100 insulin. The pump is indicated for use in individuals 6 years of age and greater.
Control-IQ technology: Control-IQ technology is intended for use with compatible integrated continuous glucose monitors (iCGM, sold separately) and alternate controller enabled (ACE) pumps to automatically increase, decrease, and suspend delivery of basal insulin based on iCGM readings and predicted glucose values. It can also deliver correction boluses when the glucose value is predicted to exceed a predefined threshold. Control-IQ technology is intended for the management of Type 1 diabetes mellitus in persons 6 years of age and greater. Control-IQ technology is intended for single patient use. Control-IQ technology is indicated for use with NovoLog or Humalog U-100 insulin.
Warning: Control-IQ technology should not be used by anyone under the age of 6 years old. It should also not be used in patients who require less than 10 units of insulin per day or who weigh less than 55 pounds.
Control-IQ technology is not indicated for use in pregnant women, people on dialysis, or critically ill patients. Do not use Control-IQ technology if using hydroxyurea. Users of a Tandem insulin pump and Control-IQ technology must use the insulin pump, CGM, and all other system components in accordance with their respective instructions for use; test blood glucose levels as recommended by their healthcare provider; maintain sufficient diabetes self-care skills; see healthcare provider(s) regularly; and have adequate vision and/or hearing to recognize all functions of the pump, including alerts, alarms, and reminders. If your CGM readings do not match your symptoms or expectations, use a blood glucose meter to make diabetes treatment decisions. The Tandem pump and the CGM transmitter and sensor must be removed before MRI, CT, or diathermy treatment. Exposure to MRI, CT, or diathermy treatment can damage the components. Visit tandemdiabetes.com/safetyinfo for additional important safety information.