Nobody likes shots. Adults don’t like giving them, and kids don’t like receiving them. Tandem insulin pumps are powered by Control-IQ+ technology — which is designed to help kids and teens stay in range.

Playtime Powered by Control-IQ+
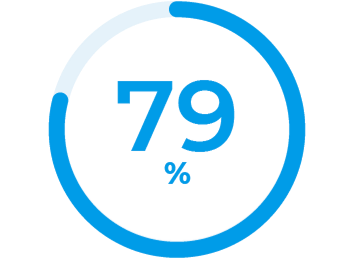
Time in Range2*
According to real-world results
Big Dreams Powered by Control-IQ+
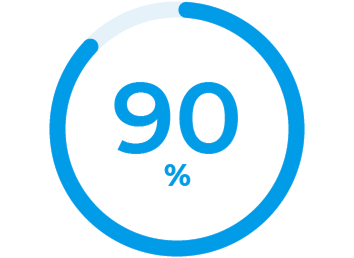
Time in Range Overnight
Real-world data demonstrated for all age groups3


Memories Powered by Control-IQ+
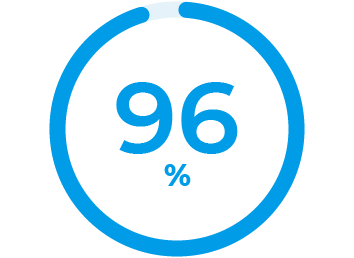
Time in Closed-Loop Automation4

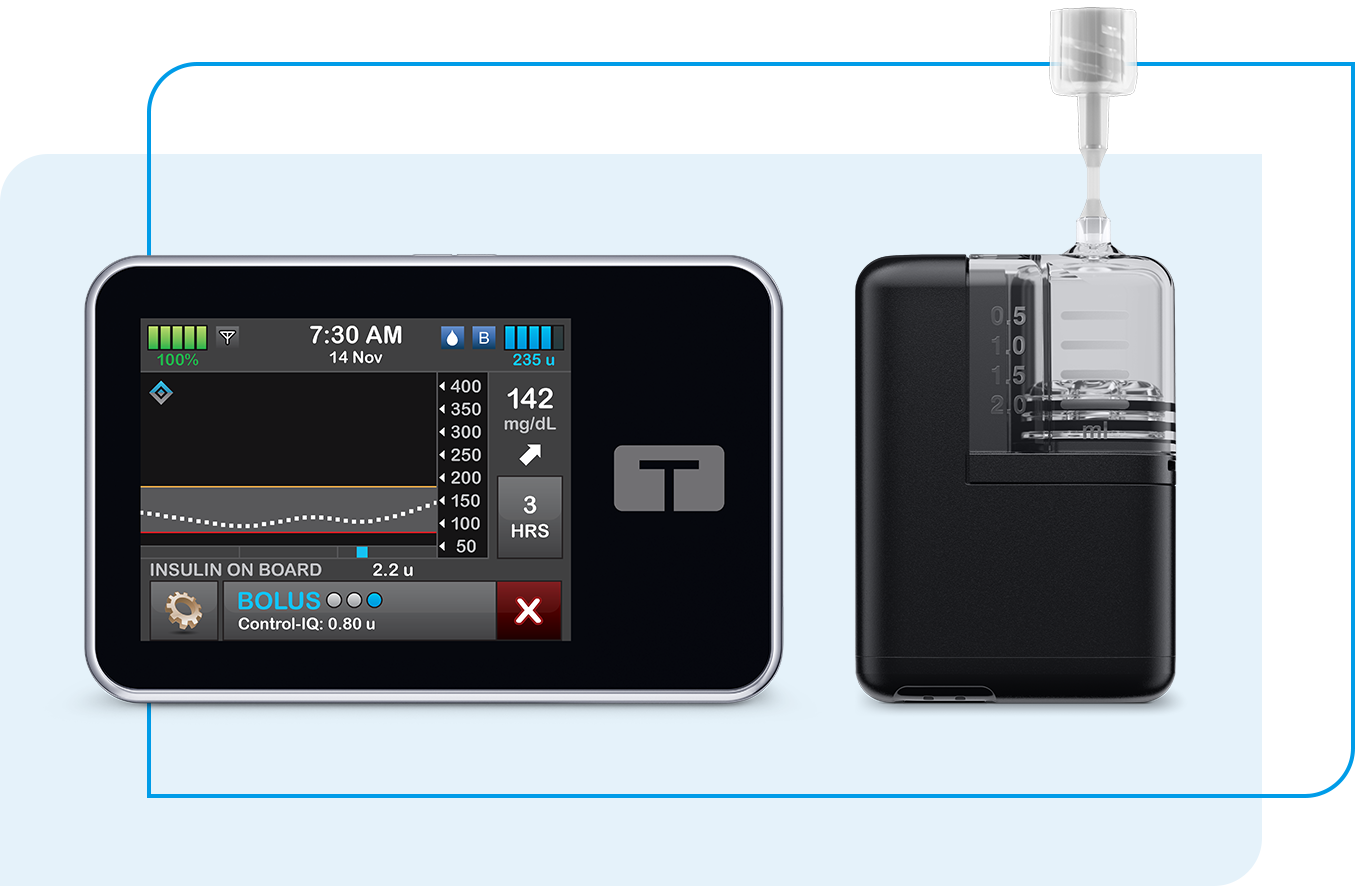
Tandem Mobi System
This insulin pump can be worn almost anywhere,† giving you more options for how you manage your diabetes. It’s powered by Control-IQ+ and is controllable with a compatible, personal iPhone.‡
Explore Pump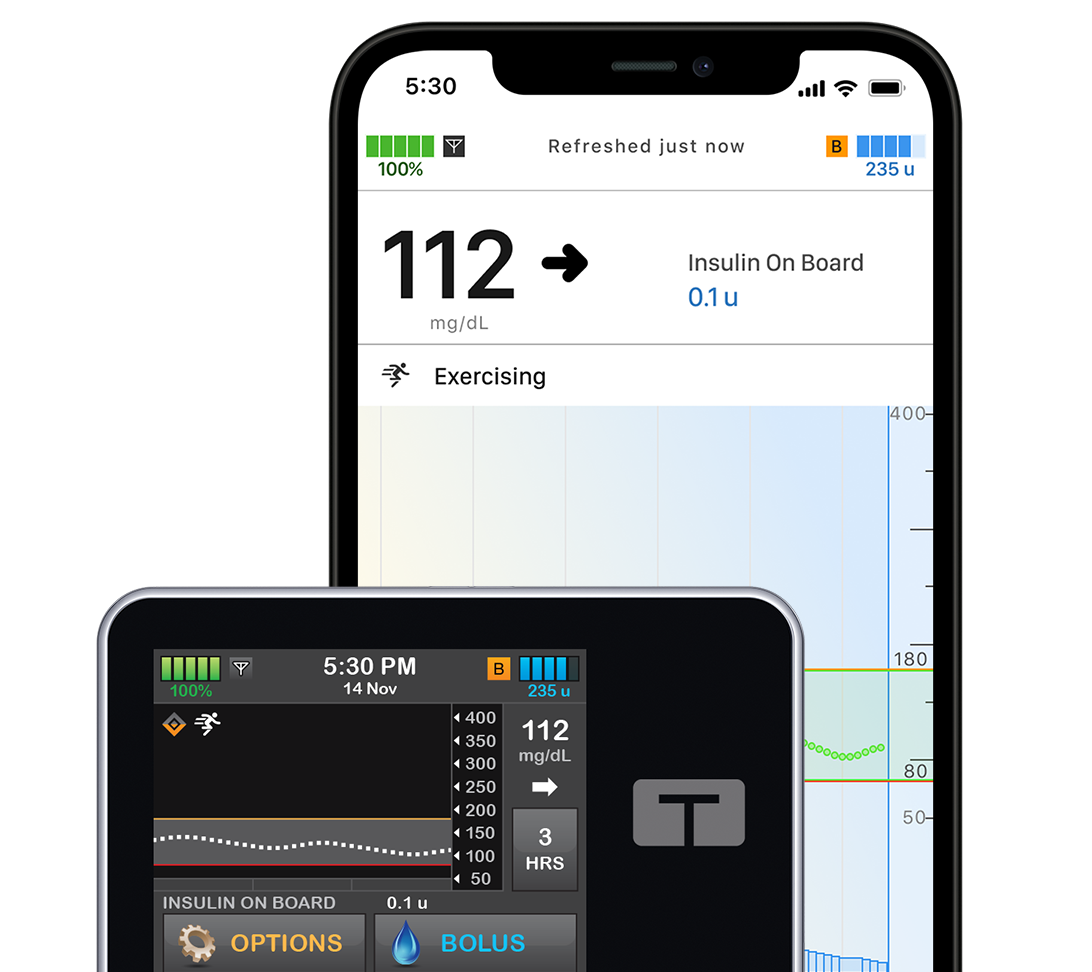
t:slim X2 Insulin Pump
Sleek and modern, this all-in-one pump is easy to use, has a color touchscreen, and it pairs with multiple CGM sensors. It's powered by Control-IQ+, which predicts and helps prevent highs and lows.
Explore PumpLife is Better with Options
Tandem pumps are compatible with multiple continuous glucose monitoring (CGM) sensors,§ so you can pick the one that best fits your family’s lifestyle.
Get started today!
A Tandem Diabetes Care Specialist will help you get started.
See the Features #TeamTandem Parents Know and Love
The Only System with AutoBolus
Better A1c results, even for kids or teens who occasionally miss meal boluses.5
Better Sleep for the Whole Family
The only system with a dedicated Sleep Activity. Data showed a 90% overnight time in range for real-world users.3
Small On-Body Footprint
More than 30 mix-and-match infusion set options for convenience, choice, and discretion.
Personal Profiles
Create up to six Personal Profiles to account for changing insulin needs (growth spurts, hormones, etc.).
Get a Tandem pump for less than you think.
The average Tandem Diabetes Care customer pays less than $50 monthly (yes, that includes supplies)!^
Whether you're ready to get an insulin pump, or looking to check insurance coverage, you’ll find everything you need here.
Get StartedWhat People Are Saying
Hear from parents how Tandem automated delivery systems have made life better for the whole family.
I'm not as worried as much as I used to be now that he uses Tandem. He can sleep through the night, which means I'm not waking up as much.
Maria
Mother to Jarim, diagnosed 2020

We started using Tandem and his A1c went down. The control was so much better compared to MDI.
Markquetto
Mother to Syncere, diagnosed 2023

Going from shots to the Tandem Mobi has been life-changing. The accuracy and control we have now has been great.
Ginny
Mother to Ben, diagnosed 2024

Raelynn loves her Tandem Mobi system. Her A1c continues to improve and we have really dialed in the settings to be exactly what her little body needs.
Shannon
Mother to Raelynn, diagnosed 2022

Individual symptoms, situations, circumstances, and results may vary.
What's next?
Whether you're ready to get a Tandem insulin pump, or looking to check insurance coverage, you’ll find everything you need here.



